Connect With Us
Featured Articles

Treatment of Toe Fractures

Fractures affecting the toes are a frequent occurrence. These fractures are often the result of crushing injuries or from stubbing the toes. While less common, joint hyperextension and stress fractures can also lead to toe fractures. Patients typically experience tenderness at the fracture site or pain when gentle pressure is applied to the affected digit. Imaging tools are valuable for identifying fractures, assessing displacement, and evaluating nearby areas and toes. There may be compromised circulation, open fractures, or significant soft tissue damage. Additionally, displaced or unstable fractures of the first toe may involve more than 25 percent of the joint surface. Stable, nondisplaced toe fractures are typically treated with buddy taping and the use of a rigid-sole shoe to restrict joint mobility. In contrast, displaced fractures of the lesser toes require reduction where the bone is manipulated back into place and buddy taping. If you have a broken toe, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment that will help relieve pain.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact one of our podiatrists from New England Foot and Ankle. Our doctors will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
Optimal Footwear Choices for Nurses on the Job

Selecting appropriate footwear is vital for nurses who spend long hours on their feet. Comfort and support are paramount to withstand the demands of the healthcare profession. A top choice for nurses is a well-cushioned, slip-resistant shoe that provides stability on various surfaces. Opting for a shoe with ample arch support can help alleviate stress on the feet, minimizing discomfort during extended shifts. Breathability is essential, and choosing shoes with moisture-wicking materials ensures a cool and dry environment for the feet. Additionally, slip-on or lace-up styles with a secure fit are practical for quick movements in fast-paced healthcare settings. Footwear brands catering specifically to healthcare professionals often integrate advanced features to address the unique challenges nurses face. Prioritizing comfort and functionality in footwear contributes significantly to the well-being of nurses and enhances their ability to deliver quality care throughout their demanding workday. If you would like more information about what type of footwear to purchase for your work day, it is suggested that you schedule an appointment with a podiatrist.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact one of our podiatrists from New England Foot and Ankle. Our doctors will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Working on Your Feet
Foot care is important regardless of your profession, but those who work on their feet must pay special attention. Bunions, calluses, blisters, and plantar warts are just a few of the many conditions that can arise after standing all day. While painful at their worst, these conditions can easily be avoided with the right foot care. This includes both appropriate footwear and proper posture—important elements that affect the health of your feet.
Choosing appropriate footwear means choosing a shoe that has a negative heel. This means that the heel is slightly lower than the ball of your foot, which places less of a strain. If you have a profession that requires you to be on your feet all day, investing in a pair of high-quality shoes is pertinent. High-quality shoes can be purchased from a respected manufacturer that emphasizes foot care and foot health.
Despite the regularity of wearing shoes, the feet are naturally not designed to be enclosed. Regular “barefoot” time for your feet can be beneficial for foot health. Among other methods, allowing your feet to breathe can help alleviate the pain and pressure your feet may be experiencing from being on your feet all day.
Simple foot exercises and yoga positions can help improve both the health and function of your feet. Active foot exercises that create movement will stimulate your foot’s blood flow and circulation, and yoga positions that place your feet flat onto the floor will stretch out their muscles. Yoga is particularly beneficial for your Achilles tendon and calf muscles, which are areas that can become especially problematic if not taken care of. Foot exercises and yoga positions can be easily performed every day at virtually any location and any time; whether it is at the office, at the gym, or at home right before you go to bed. Simple stretching can increase your foot health by miles.
The foot pain you experience after lengthy hours working on your feet may seem inevitable and unavoidable; in reality, however, that is not the case. Wearing proper footwear and performing simple foot exercises and stretches can help ease foot pain and allow you to truly avoid frustrating foot problems.
Your feet can easily be kept healthy with some education and a little effort. Pain that begins at the feet can eventually affect the whole body. Begin taking care of your feet now!
Ankle Sprains Defined by Symptoms

An ankle sprain, a common injury, manifests as the stretching or tearing of ligaments that support the ankle joint. The intricate anatomy of the ankle involves three lateral ligaments, which are the anterior talofibular, calcaneofibular, and posterior talofibular ligaments, and all are vital for stability. When subjected to excessive force, often due to sudden twists or impacts, these ligaments can undergo strain or damage, resulting in an ankle sprain. Symptoms of this injury are discernible through localized pain, swelling, and tenderness around the affected area. Individuals with an ankle sprain often experience difficulty bearing weight on the injured foot and may notice bruising. The severity of symptoms varies, ranging from mild discomfort to significant pain and functional impairment. If you have sprained your ankle, it is suggested that you visit a podiatrist who can offer the correct treatment for complete healing.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact one of our podiatrists from New England Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Three Grades of Ankle Sprains
An ankle sprain occurs when one or more ankle ligament gets overly stretched. Ligaments are strong bands of tissue that bind and support the bones and other structures that make up the ankle. In more severe ankle sprains, the ligament(s) tear—either partially or completely—and there may be an audible popping noise at the moment of injury.
Ankle sprains are quite common and can occur when the ankle rolls outwardly (eversion) or inwardly (inversion), causing the ligament(s) to stretch beyond normal limits, or even tear. Falls, twists, or blows to the ankle during sports or other activities can cause this injury, as well as wearing improper footwear, running on uneven surfaces, or having weak ankles.
Depending on the injury’s severity, an ankle sprain will be classified as Grade I, Grade II, or Grade III. Grade I sprains involve ligament(s) being overly stretched but not torn, with symptoms of mild pain, swelling, and ankle instability. There may also be some difficulty bearing weight. A Grade II sprain usually involves a partial tear of the ligament which brings more intensity in these symptoms, along with possible bruising. With a Grade III sprain, the ligament is completely torn, the symptoms are severe, and it may not be possible to put weight on the affected foot at all.
To diagnose and grade an ankle sprain, a podiatrist will perform a physical examination, checking for tenderness and range of motion in the ankle. For more severe sprains, X-rays or other imaging studies may be necessary.
It is vitally important to have an ankle sprain treated properly as improper healing often leads to future ankle sprains and possibly even chronic ankle stability. Treatment for an ankle sprain will vary, depending on its severity, and may include the RICE method (Rest/Ice/Compression/Elevation), physical therapy, bracing, medications, and possibly even surgery to repair a torn ligament. Rehabilitation is very important for the sprain to heal properly and to restore functionality.
Arthritis Can Cause Pain in the Feet and Ankles
Peripheral Artery Disease and Your Feet
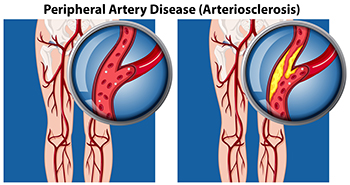
Peripheral artery disease, or PAD, is a condition that affects the arteries, causing narrowing and restricting blood flow, primarily to the lower limbs and feet. It is more prevalent among people aged 50 to 75, with more women than men affected. The hallmark symptom of PAD is intermittent pain in one or both calves during physical activity, which subsides with rest. This discomfort stems from the narrowed femoral artery, which hinders adequate delivery of blood and oxygen to calf muscles and feet during movement. Walking uphill or climbing stairs may intensify the pain. In severe cases, where blood supply is significantly reduced, individuals may experience pain, particularly at night. This type of pain typically is felt in the toes and feet. Other signs of peripheral artery disease include poor hair and toenail growth cool feet, and weak or absent pulses in the arteries of the feet. If left untreated, PAD can lead to complications such as skin ulcers and, in rare cases, gangrene. For that reason, if you believe you have developed peripheral artery disease, it is suggested that you schedule regular appointments with a podiatrist who is trained to manage symptoms effectively. A podiatrist can assess circulation, identify potential issues, and provide guidance on lifestyle modifications that can improve your overall foot health.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from New England Foot and Ankle. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Featured Articles
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- March 2016